Neurofeedback
What is Neurofeedback?
Neurofeedback is often referred to as Neurotherapy, EEG (electroencephalography) Biofeedback or simply Biofeedback. It is a much-researched, proven non-invasive treatment for a wide range of neurological conditions and disorders such as ADHD, Anxiety and PTSD found in children, teens and adults. Neurofeedback helps you to learn how to regulate brainwave activity to reduce unwanted symptoms or behaviors, so you can become the best version of you.
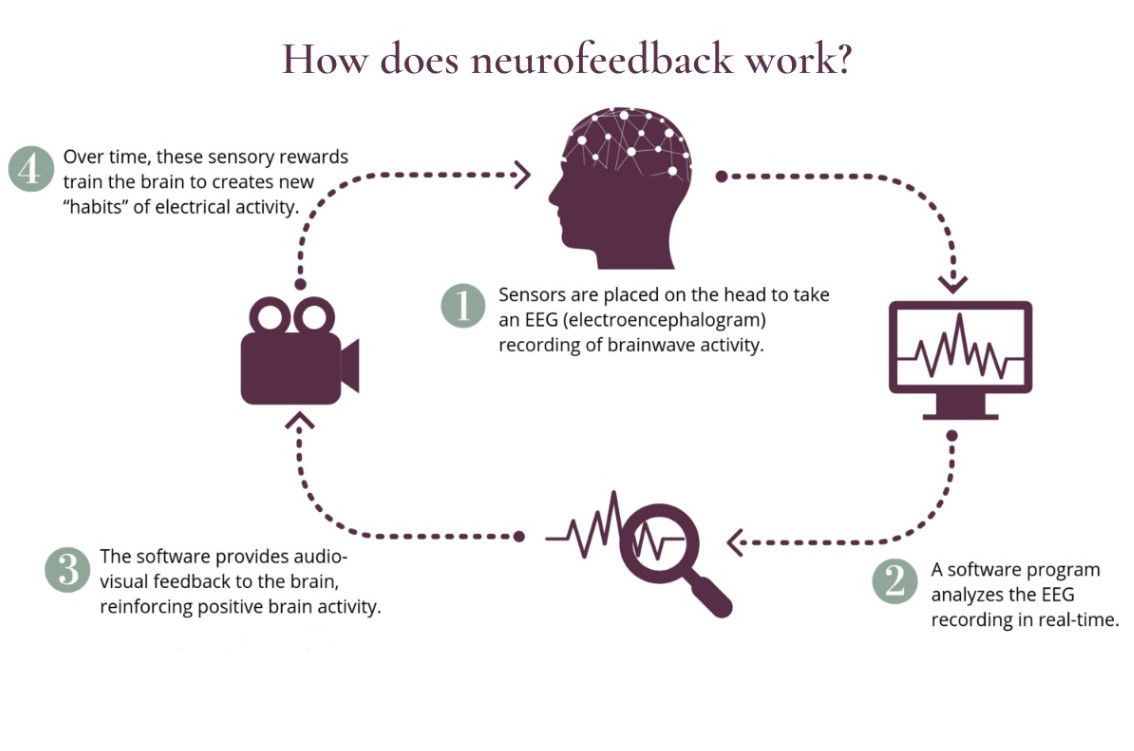
How does Neurofeedback work?
A typical neurofeedback session follows these basic steps:
- Set goals for treatment. For example, the goal of anxiety treatment may be to regulate fast brain wave activity so that a patient feels calmer and more relaxed after a session.
- A clinician starts by placing electrodes on a patient’s scalp to obtain a real-time measurement of their brain waves (i.e. electroencephalography, or EEG). No current is sent into the brain. Instead, the sensors receive cortical activity and send it to the computer. After set-up, the patient may watch a movie, play a video game, or listen to music as neurofeedback training begins.
- Train the brain with positive feedback. When the EEG detects that a patient’s brain wave activity has met the goals of treatment, the brain is rewarded with positive feedback. This may be feedback sounds or watching a screen which is brighter.
- Repeat training. The EEG continues to monitor the patient’s brain waves and give positive feedback when goals of treatment are met. This training loop gives the brain thousands of opportunities to self-correct and be rewarded in one session.
 Training the brain with positive feedback is based on the principles of learning theory, or operant conditioning, and is similar to how we train a dog to sit by rewarding it with a treat. Our brains, like animals, are constantly seeking rewards.Notably, neurofeedback does not involve any electrical current or stimulation of the brain like some other brain-based therapies (ex. TMS, LENS, or tDCS).
Training the brain with positive feedback is based on the principles of learning theory, or operant conditioning, and is similar to how we train a dog to sit by rewarding it with a treat. Our brains, like animals, are constantly seeking rewards.Notably, neurofeedback does not involve any electrical current or stimulation of the brain like some other brain-based therapies (ex. TMS, LENS, or tDCS).In a nutshell: Our brains use brain waves to communicate and function properly. These brain waves may become dysregulated, which can lead to psychiatric or neurological symptoms. Neurofeedback is a non-invasive treatment that addresses imbalances in brain wave activity to help patients achieve deeper healing and better functioning.

Neurofeedback is not considered a cure, but rather a method of managing or regulating the workings of the brain so it functions in a healthier manner. This is achieved by repeated training sessions using a computerized neurofeedback program that teaches your central nervous system to reorganize and regulate brainwave frequencies. Neurofeedback assesses your brain and provides information about areas of dysfunction that are causing symptoms so that they can be treated directly. Various neurofeedback methods and equipment are used for different types of neurological problems.
Why Neurofeedback?
Neurofeedback is painless, drug-free, has no know side effects and is long lasting.
Medications for conditions such as ADHD, Anxiety and PTSD provide regulation with symptom relief while the medication is being taken. Regulation learned with Neurofeedback is long lasting which helps to reduce or remove undesirable symptoms and behaviors long term (Arnold et al 2021; Becerra et al 2006; Dobrakowski, et al , 2020; Kouijzer et al, 2009). Through Neurofeedback the connections in the brain are completely re-wired as a result of our brain’s ability to change, called Neuroplasticity.
14.4% of Israeli Children are diagnosed with ADHD, compared to 6.8% average worldwide (Davidovitch et al, 2017).
References
Arnold, L. E., Arns, M., Barterian, J., Bergman, R., Black, S., Conners, C. K., ... & Williams, C. E. (2021). Double-blind placebo-controlled randomized clinical trial of neurofeedback for attention-deficit/hyperactivity disorder with 13-month follow-up. Journal of the American Academy of Child & Adolescent Psychiatry, 60(7), 841-855.
Becerra, J., Fernandez, T., Harmony, T., Caballero, M. I., Garcia, F., Fernandez-Bouzas, A., ... & Prado-Alcalá, R. A. (2006). Follow-up study of learning-disabled children treated with neurofeedback or placebo. Clinical EEG and neuroscience, 37(3), 198-203.
Dobrakowski, P., & Łebecka, G. (2020). Individualized neurofeedback training may help achieve long-term improvement of working memory in children with ADHD. Clinical eeg and Neuroscience, 51(2), 94-101.
Kouijzer, M. E., de Moor, J. M., Gerrits, B. J., Buitelaar, J. K., & van Schie, H. T. (2009). Long-term effects of neurofeedback treatment in autism. Research in Autism Spectrum Disorders, 3(2), 496-501.
Medications for conditions such as ADHD, Anxiety and PTSD provide regulation with symptom relief while the medication is being taken. Regulation learned with Neurofeedback is long lasting which helps to reduce or remove undesirable symptoms and behaviors long term (Arnold et al 2021; Becerra et al 2006; Dobrakowski, et al , 2020; Kouijzer et al, 2009). Through Neurofeedback the connections in the brain are completely re-wired as a result of our brain’s ability to change, called Neuroplasticity.
14.4% of Israeli Children are diagnosed with ADHD, compared to 6.8% average worldwide (Davidovitch et al, 2017).
References
Arnold, L. E., Arns, M., Barterian, J., Bergman, R., Black, S., Conners, C. K., ... & Williams, C. E. (2021). Double-blind placebo-controlled randomized clinical trial of neurofeedback for attention-deficit/hyperactivity disorder with 13-month follow-up. Journal of the American Academy of Child & Adolescent Psychiatry, 60(7), 841-855.
Becerra, J., Fernandez, T., Harmony, T., Caballero, M. I., Garcia, F., Fernandez-Bouzas, A., ... & Prado-Alcalá, R. A. (2006). Follow-up study of learning-disabled children treated with neurofeedback or placebo. Clinical EEG and neuroscience, 37(3), 198-203.
Dobrakowski, P., & Łebecka, G. (2020). Individualized neurofeedback training may help achieve long-term improvement of working memory in children with ADHD. Clinical eeg and Neuroscience, 51(2), 94-101.
Kouijzer, M. E., de Moor, J. M., Gerrits, B. J., Buitelaar, J. K., & van Schie, H. T. (2009). Long-term effects of neurofeedback treatment in autism. Research in Autism Spectrum Disorders, 3(2), 496-501.
What to Expect
While you relax in a chair, sensors will be attached to your scalp. A computer EEG program will process your brain signals and provide information about various brainwave frequencies. Using a program you will watch graphics and listen to sounds which provide your brain and central nervous system with feedback signals from the program. The program will then begin directing your brainwave activity toward more desirable and controlled patterns. You will get immediate feedback from the program when your brainwave patterns improve. Between sessions, you should be able to notice changes in stress, sleep patterns, or mental clarity.


How many treatments do I need?
Treatment length ranges between 40-60 mins depending on the age of the client. The average amount of treatments range between 20 - 40. After 20 treatments the progression is tracked. For severe dysregulation, the amount of treatments can reach up to 80.
For the quickest best results treatments are given twice weekly. I like to compare this to going to the gym. Just as a body builder cannot train the muscles in the body to grow once a week, the brain muscle also needs to be taught at least twice a week for it to strengthen.
For the quickest best results treatments are given twice weekly. I like to compare this to going to the gym. Just as a body builder cannot train the muscles in the body to grow once a week, the brain muscle also needs to be taught at least twice a week for it to strengthen.
Neurofeedback and Attention Deficit Hyperactivity Disorder (ADHD)
Attention-Deficit/Hyperactivity Disorder (ADHD):
Attention-deficit/hyperactivity disorder (ADHD) is a brain-based disorder marked by an ongoing pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development.
The most common form of treating ADHD/ADD symptoms is medication; however, it only provides temporary relief from the symptoms and when stopped the symptoms return.
An alternative or conjunctive to medication is Neurofeedback. Neurofeedback aims to train the brain’s attention networks to function better and correct the root of the problem – brainwave dysregulation. There are many studies that show that the brain is capable of change and can reorganize brainwave patterns to a more optimal state reducing symptoms through consistent practice. Neurofeedback strengthens attention networks so a patient can improve concentration, focus, and sustain attention.
Also, neurofeedback training has been commonly found to be associated with decreased impulsiveness and hyperactivity, increased mood stability, improved sleep patterns, and increased attention span.
Research:
The Brain Map below shows that a normalized brain (left image) will show a green or “normalized” state of “0”. A patient that exhibits ADHD symptoms (right image) will show a red frontal lobe indicating brainwave dysregulation. Research has shown that in this particular image that this is due to a higher level of theta brain waves in the frontal lobe and the dysregulation produces inattention, lack of concentration and focus that pertains to those experiencing ADHD symptoms.

Fuchs, et. al. (2003) demonstrated that neurofeedback produced comparable improvements to Ritalin. In a one-year follow-up, control group study, Monastra et al. (2002) found that neurofeedback produced superior improvements to Ritalin, without needing to remain on medication.
Since the late 1970’s, neurofeedback has been researched, refined, and tested with ADHD. Clinical work by Dr. Lubar and his colleagues at the University of Tennessee demonstrated that it is possible to retrain the brain with neurofeedback. Neurofeedback research is quite strong in demonstrating its effectiveness in treating ADHD, whereas the average stimulation medication study follow-up is only three weeks long and the longest medication study is only 14 months long with ADHD. Dr. Lubar (1995) published a 10-year follow-ups on cases and found that in approximately 80% of patients, neurofeedback substantially improved the symptoms of ADHD, and these changes were maintained.
References
Fuchs, T., Birbaumer, N., Lutzenberger, W., Gruzelier, J. H., & Kaiser, J. (2003). Neurofeedback treatment for attention-deficit/hyperactivity disorder in children: a comparison with methylphenidate. Applied psychophysiology and biofeedback, 28(1), 1-12.
Lubar, J. F. (1995). Neurofeedback for the management of attention-deficit/hyperactivity disorders. Chapter in M. S. Schwartz (Ed.), Biofeedback: A Practitioner's Guide. New York, Guilford, 493-522.
Monastra, V. J., Monastra, D. M., & George, S. (2002). The effects of stimulant therapy, EEG biofeedback, and parenting style on the primary symptoms of attention-deficit/hyperactivity disorder. Applied psychophysiology and biofeedback, 27(4), 231-249.
Attention-deficit/hyperactivity disorder (ADHD) is a brain-based disorder marked by an ongoing pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development.
- Inattention – A person has difficulty sustaining focus, disorganized; these problems are not due to defiance or lack of comprehension.
- Hyperactivity – A person seems to move constantly, excessively fidgets, taps, or talks incessantly, including situations that are not considered appropriate. In adults, it may be extreme restlessness or wearing others out with constant activity.
- Impulsivity – A person who makes actions in the moment without considering long-term consequences; or showing a desire for immediate rewards or inability to delay gratification. An impulsive person may be socially intrusive or excessively interrupt others.
The most common form of treating ADHD/ADD symptoms is medication; however, it only provides temporary relief from the symptoms and when stopped the symptoms return.
An alternative or conjunctive to medication is Neurofeedback. Neurofeedback aims to train the brain’s attention networks to function better and correct the root of the problem – brainwave dysregulation. There are many studies that show that the brain is capable of change and can reorganize brainwave patterns to a more optimal state reducing symptoms through consistent practice. Neurofeedback strengthens attention networks so a patient can improve concentration, focus, and sustain attention.
Also, neurofeedback training has been commonly found to be associated with decreased impulsiveness and hyperactivity, increased mood stability, improved sleep patterns, and increased attention span.
Research:
The Brain Map below shows that a normalized brain (left image) will show a green or “normalized” state of “0”. A patient that exhibits ADHD symptoms (right image) will show a red frontal lobe indicating brainwave dysregulation. Research has shown that in this particular image that this is due to a higher level of theta brain waves in the frontal lobe and the dysregulation produces inattention, lack of concentration and focus that pertains to those experiencing ADHD symptoms.
Fuchs, et. al. (2003) demonstrated that neurofeedback produced comparable improvements to Ritalin. In a one-year follow-up, control group study, Monastra et al. (2002) found that neurofeedback produced superior improvements to Ritalin, without needing to remain on medication.
Since the late 1970’s, neurofeedback has been researched, refined, and tested with ADHD. Clinical work by Dr. Lubar and his colleagues at the University of Tennessee demonstrated that it is possible to retrain the brain with neurofeedback. Neurofeedback research is quite strong in demonstrating its effectiveness in treating ADHD, whereas the average stimulation medication study follow-up is only three weeks long and the longest medication study is only 14 months long with ADHD. Dr. Lubar (1995) published a 10-year follow-ups on cases and found that in approximately 80% of patients, neurofeedback substantially improved the symptoms of ADHD, and these changes were maintained.
References
Fuchs, T., Birbaumer, N., Lutzenberger, W., Gruzelier, J. H., & Kaiser, J. (2003). Neurofeedback treatment for attention-deficit/hyperactivity disorder in children: a comparison with methylphenidate. Applied psychophysiology and biofeedback, 28(1), 1-12.
Lubar, J. F. (1995). Neurofeedback for the management of attention-deficit/hyperactivity disorders. Chapter in M. S. Schwartz (Ed.), Biofeedback: A Practitioner's Guide. New York, Guilford, 493-522.
Monastra, V. J., Monastra, D. M., & George, S. (2002). The effects of stimulant therapy, EEG biofeedback, and parenting style on the primary symptoms of attention-deficit/hyperactivity disorder. Applied psychophysiology and biofeedback, 27(4), 231-249.
Neurofeedback and Anxiety
Anxiety disorders come in many forms. A main trigger is a person’s tolerance level and response to stress/stressors. Anxiety is a common response to stress with sufferers often felt overwhelmed, exhausted, and fatigued. It can manifest through physical, psychological, dietary, or environmental sources. When a person develops a pattern of over thinking, the brain will respond with physical and psychological symptoms. This can be very difficult to break and can develop into a chronic pattern affecting a person’s daily life. Anxiety can manifest to the point that it interrupts normal sleep patterns and negatively influences quality of life.
Many sufferers often feel they are unable to concentrate and are plagued by constant fatigue and stress. Some suffers show symptoms through physical symptoms; such as headaches, nervousness, nail-biting, sweating, and restlessness. Many internalize their symptoms and experience a lack of focus, poor concentration, and/or poor short or long-term memory. These types of sufferers may outwardly appear calm but their mind is constantly racing and ruminating over specific things or events (past and future). Many have a difficult time living in the present and constantly worry about past mistakes or future problems.
This can happen at any age but children and teens usually do not have the maturity to fully grasp how to communicate or express their feelings. Behavior or mood changes can occur, acting-out, and depression are common responses as well.
Common Anxiety Disorder Symptoms include:
How can Neurofeedback help Anxiety Disorders?
Neurofeedback trains brainwaves based on a psychological process called operant conditioning. We aim to retrain these brainwave patterns by using positive reinforcement to teach the brain to make new connections and rework disorganized brainwave patterns. With consistent practice, neurofeedback will provide the opportunity for the brain to balance appropriately and symptom responses to stress and anxiety should improve. The brain develops the skills needed to reduce anxiety in their lives.
Those that are regularly prescribed anti-anxiety medications aim to ease the negative symptoms; however, once these prescription drugs are stopped, symptoms will return. As the brain retrains with neurofeedback to decrease anxiety and learns to remain more calm, often less medication is needed. Neurofeedback, in conjunction with cognitive behavioral therapy or other behavioral tools, work best to help eliminate anxiety and improve one's daily functioning and promote a better quality of life. Overall, neurofeedback has been proven to help reduce many mental health concerns long term and aides in the process to help those looking to wean off medication with their doctor’s supervision. Be mindful that some may have to take medication long term due to physiological reasons.
References
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR™)(2022).American Psychiatric Association. http://dsm.psychiatryonline.org.
Many sufferers often feel they are unable to concentrate and are plagued by constant fatigue and stress. Some suffers show symptoms through physical symptoms; such as headaches, nervousness, nail-biting, sweating, and restlessness. Many internalize their symptoms and experience a lack of focus, poor concentration, and/or poor short or long-term memory. These types of sufferers may outwardly appear calm but their mind is constantly racing and ruminating over specific things or events (past and future). Many have a difficult time living in the present and constantly worry about past mistakes or future problems.
This can happen at any age but children and teens usually do not have the maturity to fully grasp how to communicate or express their feelings. Behavior or mood changes can occur, acting-out, and depression are common responses as well.
Common Anxiety Disorder Symptoms include:
- Excessive worry or nervousness
- Trouble concentrating or focusing on anything other than the present worry.
- Heightened fear or feeling powerless
- Restlessness
- Separation anxiety disorder is a childhood disorder characterized by anxiety that is excessive for the developmental level and related to separation from parents or others who have parental roles.
- Selective mutism is a consistent failure to speak in certain situations, such as school, even when you can speak in other situations, such as at home with close family members. This can interfere with school, work and social functioning.
- Specific phobias are characterized by major anxiety when you’re exposed to a specific object or situation and a desire to avoid it. Phobias provoke panic attacks in some people.
- Social anxiety disorder (social phobia) involves high levels of anxiety, fear and avoidance of social situations due to feelings of embarrassment, self-consciousness and concern about being judged or viewed negatively by others.
- Panic disorder involves repeated episodes of sudden feelings of intense anxiety and fear or terror that reach a peak within minutes (panic attacks). You may have feelings of impending doom, shortness of breath, heart palpitations or chest pain.
- Agoraphobia is anxiety about, and often avoidance of, places or situations where you might feel trapped or helpless if you start to feel panicky or experience embarrassing symptoms, such as losing control.
- Generalized anxiety disorder includes persistent and excessive anxiety and worries about activities or events — even ordinary, routine issues. The worry is usually out of proportion to the actual circumstance, is difficult to control and interferes with your ability to focus on current tasks. It often occurs along with other anxiety disorders or depression.
- Substance-induced anxiety disorder is characterized by prominent symptoms of anxiety or panic that are a direct result of abusing drugs, taking medications, being exposed to a toxic substance or withdrawal from drugs.
- Anxiety disorder due to a medical condition includes prominent symptoms of anxiety or panic that are directly caused by a physical health problem.
- Specified anxiety disorder and unspecified anxiety disorder are terms for anxiety or phobias that don’t meet the exact criteria for any other anxiety disorders but are significant enough to be distressing and disruptive.
How can Neurofeedback help Anxiety Disorders?
Neurofeedback trains brainwaves based on a psychological process called operant conditioning. We aim to retrain these brainwave patterns by using positive reinforcement to teach the brain to make new connections and rework disorganized brainwave patterns. With consistent practice, neurofeedback will provide the opportunity for the brain to balance appropriately and symptom responses to stress and anxiety should improve. The brain develops the skills needed to reduce anxiety in their lives.
Those that are regularly prescribed anti-anxiety medications aim to ease the negative symptoms; however, once these prescription drugs are stopped, symptoms will return. As the brain retrains with neurofeedback to decrease anxiety and learns to remain more calm, often less medication is needed. Neurofeedback, in conjunction with cognitive behavioral therapy or other behavioral tools, work best to help eliminate anxiety and improve one's daily functioning and promote a better quality of life. Overall, neurofeedback has been proven to help reduce many mental health concerns long term and aides in the process to help those looking to wean off medication with their doctor’s supervision. Be mindful that some may have to take medication long term due to physiological reasons.
References
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR™)(2022).American Psychiatric Association. http://dsm.psychiatryonline.org.
Neurofeedback and Post Traumatic Stress Disorder (PTSD)
Patients with trauma or PTSD often wonder why they can’t move on from past events, even if they happened years ago. Through talk therapy, they may come to understand that they are no longer in danger, yet may continue to experience heightened anxiety, panic, flashbacks and nightmares. This is because trauma affects more than just our thoughts. Trauma changes the brain and body in ways that talking and reasoning may not be able to reverse. Healing from trauma requires healing the brain and body’s biology, not just our thoughts.
Neurofeedback is one of the new promising, evidence-based therapies that can help address the deeper, underlying biological changes that result from trauma and PTSD.
“THE BODY KEEPS SCORE”: TRAUMA & THE BODY
During a traumatic event, the amygdala alerts the hypothalamus, a part of the brain that coordinates the body’s stress response by producing hormones like cortisol. In addition, the autonomic nervous system - which controls our involuntary body functions - goes into fight, flight or freeze mode. This means having a faster heart rate, breathing more shallowly, sweating, and not being able to think clearly. In this way, trauma can change the body’s biology. Even after the trigger is gone, the amygdala can hold onto the physical memory of trauma, and our bodies can get stuck in this fight-or-flight mode, leaving us with higher levels of cortisol and symptoms of hyperarousal.
Treatment
While we can ask someone to calm down and think more rationally, that may not change their whole-body response to trauma. We need trauma treatments that can heal the brain and body’s biology.
“Traditionally we’ve tried to heal PTSD through talking and making meaning of the event, but treatment methods that help calm arousal systems in the deeper regions of the brain have been helpful in calming PTSD more than those that try to do so through talking and reasoning.” (Van der Kolk, 2014)
Does neurofeedback therapy help with trauma? What’s the evidence?
The goal of trauma-focused neurofeedback is to help shift people from a hyper-aroused state to a calmer one so that they can experience a sense of safety and react more appropriately to everyday events.
There have been many studies showing that neurofeedback can help with symptoms of PTSD. Some have even shown that neurofeedback can change brain function of PTSD patients on imaging or fMRI (Gapen et al, 2016)
Furthermore, the level of symptom improvement in most of these studies has been significant. In fact, the effect size with neurofeedback in many studies has been greater than any medication used for PTSD.
References
Van der Kolk, B (2015). A. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. New York, New York: Penguin Books,
Gapen, M., van der Kolk, B. A., Hamlin, E., Hirshberg, L., Suvak, M., & Spinazzola, J. (2016). A pilot study of neurofeedback for chronic PTSD. Applied psychophysiology and biofeedback, 41(3), 251-261.
Neurofeedback is one of the new promising, evidence-based therapies that can help address the deeper, underlying biological changes that result from trauma and PTSD.
“THE BODY KEEPS SCORE”: TRAUMA & THE BODY
During a traumatic event, the amygdala alerts the hypothalamus, a part of the brain that coordinates the body’s stress response by producing hormones like cortisol. In addition, the autonomic nervous system - which controls our involuntary body functions - goes into fight, flight or freeze mode. This means having a faster heart rate, breathing more shallowly, sweating, and not being able to think clearly. In this way, trauma can change the body’s biology. Even after the trigger is gone, the amygdala can hold onto the physical memory of trauma, and our bodies can get stuck in this fight-or-flight mode, leaving us with higher levels of cortisol and symptoms of hyperarousal.
Treatment
While we can ask someone to calm down and think more rationally, that may not change their whole-body response to trauma. We need trauma treatments that can heal the brain and body’s biology.
“Traditionally we’ve tried to heal PTSD through talking and making meaning of the event, but treatment methods that help calm arousal systems in the deeper regions of the brain have been helpful in calming PTSD more than those that try to do so through talking and reasoning.” (Van der Kolk, 2014)
Does neurofeedback therapy help with trauma? What’s the evidence?
The goal of trauma-focused neurofeedback is to help shift people from a hyper-aroused state to a calmer one so that they can experience a sense of safety and react more appropriately to everyday events.
There have been many studies showing that neurofeedback can help with symptoms of PTSD. Some have even shown that neurofeedback can change brain function of PTSD patients on imaging or fMRI (Gapen et al, 2016)
Furthermore, the level of symptom improvement in most of these studies has been significant. In fact, the effect size with neurofeedback in many studies has been greater than any medication used for PTSD.
References
Van der Kolk, B (2015). A. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. New York, New York: Penguin Books,
Gapen, M., van der Kolk, B. A., Hamlin, E., Hirshberg, L., Suvak, M., & Spinazzola, J. (2016). A pilot study of neurofeedback for chronic PTSD. Applied psychophysiology and biofeedback, 41(3), 251-261.
Neurofeedback for Autism Spectrum Disorder (ASD)
Autism Spectrum Disorder (ASD) is the name for what were previously known as four separate disorders including autistic disorder (autism) and Asperger’s disorder. ASD is a complex condition with a complex diagnosis process involving a lot of interpretation and judgment. ASD often co-exists with other diagnoses (called comorbidity by doctors). There is a striking overlap between AD/HD and ASD symptoms, which causes confusion among families, as well as professionals. When a child is distracted and moves a lot at school or has difficulties keeping focused during a conversation, people often think of AD/HD. However, these symptoms might be confused with ASD symptoms. The first case study applying Neurofeedback to autism was in 1994, 20 years after it was first seen to reduce hyperactivity and led to the significant body of evidence for Neurofeedback for ADHD. Since then the evidence has grown, as described in this free report on Neurofeedback for ASD.
Although the evidence for ASD is still building compared with ADHD, we anticipate that before too long, Neurofeeedback will be embraced as the treatment of choice for ASD.
Research Autism has an excellent summary of Neurofeedback, and an extensive summary of peer-reviewed studies on Neurofeedback for ASD.
An example of such studies are Kouijzer et al (2010) found significant improvements in reciprocal social interactions and communication skills. EEG analysis showed 60% reduced Theta waves in anterior cingulate cortex (ACC) known to be involved in social & executive dysfunctions in autism: Also a study by Coben and Padolsky (2007) found an 89% success rate improving ASD symptoms, 40% reduction in core ASD symptomatology (ATEC scores) and 76% reduction in hyper-connectivity:
References
Kouijzer, M. E., van Schie, H. T., de Moor, J. M., Gerrits, B. J., & Buitelaar, J. K. (2010). Neurofeedback treatment in autism. Preliminary findings in behavioral, cognitive, and neurophysiological functioning. Research in Autism Spectrum Disorders, 4(3), 386-399.
Coben, R., & Padolsky, I. (2007). Assessment-guided neurofeedback for autistic spectrum disorder. Journal of Neurotherapy, 11(1), 5-23.
A further 2009 study showed that the effects lasted beyond 12 months:
Although the evidence for ASD is still building compared with ADHD, we anticipate that before too long, Neurofeeedback will be embraced as the treatment of choice for ASD.
Research Autism has an excellent summary of Neurofeedback, and an extensive summary of peer-reviewed studies on Neurofeedback for ASD.
An example of such studies are Kouijzer et al (2010) found significant improvements in reciprocal social interactions and communication skills. EEG analysis showed 60% reduced Theta waves in anterior cingulate cortex (ACC) known to be involved in social & executive dysfunctions in autism: Also a study by Coben and Padolsky (2007) found an 89% success rate improving ASD symptoms, 40% reduction in core ASD symptomatology (ATEC scores) and 76% reduction in hyper-connectivity:
References
Kouijzer, M. E., van Schie, H. T., de Moor, J. M., Gerrits, B. J., & Buitelaar, J. K. (2010). Neurofeedback treatment in autism. Preliminary findings in behavioral, cognitive, and neurophysiological functioning. Research in Autism Spectrum Disorders, 4(3), 386-399.
Coben, R., & Padolsky, I. (2007). Assessment-guided neurofeedback for autistic spectrum disorder. Journal of Neurotherapy, 11(1), 5-23.
A further 2009 study showed that the effects lasted beyond 12 months: